
Key Takeaways
- Sleep dentistry offers multiple sedation options to help patients manage fear and anxiety during dental procedures.
- It can be highly effective for those with dental phobias, past traumatic experiences, or sensitive gag reflexes.
- Sedation dentistry differs from general anesthesia — it keeps patients relaxed and partially conscious, allowing for a faster recovery.
- Not all sedation methods involve actual sleep; many patients remain responsive but calm.
- Understanding the difference between sedation and general anesthesia is crucial for informed decision-making.
Can sleep dentistry really eliminate fear at the dentist’s office?
Picture this: you haven’t seen a dentist in years because the very idea floods you with anxiety. Maybe it's the sound of the drill, the smell of antiseptic, or the memory of a past procedure gone wrong. For patients like you, sleep dentistry can feel like a miracle — but can it really eliminate fear?
What is sleep dentistry?
Contrary to the name, sleep dentistry doesn’t always mean you’re fully asleep. It's a term used to describe various sedation techniques that help reduce awareness, anxiety, and discomfort during dental treatment. These methods range from mild relaxation to deep sedation.
Common methods include:
- Oral sedation: Taken in pill form (e.g., triazolam), this method induces drowsiness and relaxation.
- Nitrous oxide (laughing gas): A mild sedative inhaled through a mask; wears off quickly.
- IV sedation: Delivered intravenously, this offers more profound sedation and amnesia of the procedure.
- General anesthesia: Reserved for complex surgeries or extreme anxiety; renders the patient entirely unconscious (more on this later).
Tangible outcomes: Does it reduce fear?
Yes — but results vary by individual. Many patients report complete elimination of fear, particularly when IV sedation is used. They often recall little to nothing of the procedure, which helps break the cycle of avoidance.
What the professionals say
Dr. Amir Guorgui, BSC, DMD, MACSD — a certified sedation dentist — emphasizes:
"Fear is one of the most common reasons patients avoid treatment. Sedation, especially IV or oral, creates a safe space where they can get the care they need without trauma or distress."Dr. James C.H. Ko, DDS, adds:
"For patients with anxiety or special healthcare needs, sedation dentistry is often the only way to provide effective treatment. It’s not just about comfort — it’s about access."
What is sedation dentistry, and who is it best suited for?
Sedation dentistry refers to the use of medication to help patients relax during dental procedures. Unlike general anesthesia, which induces complete unconsciousness, sedation keeps the patient in a relaxed but responsive state.
Suitable patient types
Sedation dentistry is highly beneficial for:
- Patients with moderate to severe dental anxiety
- Individuals with a low pain threshold or a high gag reflex
- Children or patients with developmental or sensory disorders
- Those requiring multiple or complex procedures in one visit
- Patients with a history of traumatic dental experiences
Types of sedation used
Sedation comes in four levels:
- Minimal sedation: You’re awake but relaxed (e.g., nitrous oxide)
- Moderate sedation (conscious sedation): You may slur words or not remember much (e.g., oral sedation)
- Deep sedation: On the edge of consciousness, but can be awakened (IV sedation)
- General anesthesia: Fully unconscious — used rarely in dental clinics
Step-by-step: How sedation dentistry works
- Initial consultation: Patient’s health, medications, and anxiety levels are assessed.
- Treatment planning: Sedation level is matched to the procedure and the patient’s needs.
- Sedation day prep: Patients are advised on fasting, accompaniment, and aftercare.
- Administration: Sedation is administered at the clinic by certified professionals.
- Monitoring: Vitals are closely monitored throughout.
- Post-treatment recovery: Patients recover in the office and are guided home safely.
<img alt="Dentist consulting with an adult woman about different dental sedation techniques src=" media="" uploads="" 2025="" 12="" 15="" types-of-dental-sedation-consultation.jpg"="">
What makes sedation dentistry different from general anesthesia?
These two are often confused — and for good reason. Both reduce awareness during procedures, but the differences are critical for safety, recovery, and application.
Key differences at a glance
| Feature | Sedation Dentistry | General Anesthesia |
|---|---|---|
| Consciousness | Patient remains conscious or semi-conscious | Fully unconscious |
| Delivery Method | Oral, inhalation, or IV | IV or gas (in hospital setting) |
| Monitoring Required | Moderate (oxygen, pulse, BP) | Intensive (hospital-grade) |
| Used For | Moderate procedures, anxiety | Complex surgeries, severe phobia |
| Recovery Time | Quick (minutes to hours) | Longer (hours, possible grogginess) |
| Side Effects | Mild nausea, drowsiness | Higher risk of complications |
| Provider Requirement | Certified sedation dentist | Anesthesiologist or oral surgeon |
Recovery and safety profile
Sedation dentistry is considered low-risk when administered by a qualified provider. Side effects are usually minor, such as:
- Dry mouth
- Mild nausea
- Brief memory gaps
By contrast, general anesthesia carries higher risks — including breathing complications and prolonged grogginess — and is only used when necessary.
When is general anesthesia appropriate?
- For patients with severe cognitive disabilities
- For lengthy reconstructive procedures (e.g., full-mouth restoration)
- When sedation fails to control movement or anxiety adequately
In Canada, general anesthesia in dental offices is highly regulated and typically offered only in hospital settings.
How does IV sedation work during a dental procedure?
Mechanism of IV sedation
Intravenous (IV) sedation involves administering sedative medication directly into the bloodstream through a vein, typically in the arm or hand. The medication used is often a benzodiazepine such as midazolam or diazepam, which acts on the central nervous system to produce calming effects.
Once administered, it induces a state of deep relaxation, where the patient is technically awake but largely unaware of the procedure. IV sedation is classified as conscious sedation — meaning the patient can respond to verbal cues or gentle touch, but often has no memory of the treatment afterward.
Administration and monitoring
- A licensed sedation dentist or anesthesiologist inserts the IV line.
- Sedative dosage is tailored to the patient's age, weight, and health status.
- Throughout the procedure, vital signs — including blood pressure, oxygen levels, and heart rate — are continuously monitored.
Effects and onset speed
The effects of IV sedation begin within 1–2 minutes of administration, making it one of the fastest-acting forms of dental sedation.
Patients typically experience:
- Euphoria or lightheadedness
- Decreased perception of time
- No recollection of sights, sounds, or sensations
Recovery can take a few hours, during which the patient should not drive or operate machinery.
Who is IV sedation for?
This method is ideal for:
- Patients with extreme dental phobia
- Those undergoing long or multiple procedures
- Individuals with strong gag reflexes or difficulty staying still
- Patients who’ve had traumatic past dental experiences
Specification table for IV sedation
| Factor | IV Sedation Details |
|---|---|
| Delivery | Intravenous injection |
| Onset Time | 1–2 minutes |
| Consciousness | Conscious but deeply relaxed |
| Memory of Procedure | Usually none |
| Monitoring | Continuous (BP, oxygen, heart rate) |
| Used For | Anxiety, lengthy procedures, gag reflex |
| Recovery Time | 2–6 hours (no driving post-procedure) |
| Risks |
What types of sedation are available for dental treatments?
Modern dentistry offers a spectrum of sedation types to suit various patient needs. From mild anxiety to complex surgical work, there's an option to match the level of comfort required.
Main types of dental sedation
- Oral Sedation
- Pills like diazepam or triazolam
- Effects begin within 30–60 minutes.
- Moderate relaxation; patient remains awake
- Nitrous Oxide (Inhalation Sedation)
- "Laughing gas" is inhaled through a nose mask.
- Fast onset; wears off quickly
- Mild sedation is excellent for children.
- IV Sedation
- Deep relaxation with little memory of the procedure
- Administered and monitored by professionals
- Conscious Sedation
- An umbrella term for techniques where the patient is still responsive
- Can be achieved via oral, inhalation, or IV methods
Intensity levels
| Sedation Type | Level of Sedation | Patient Awareness | Use Cases |
|---|---|---|---|
| Nitrous Oxide | Minimal | Fully aware | Mild anxiety, children |
| Oral Sedation | Moderate | Drowsy but conscious | Adults with moderate fear |
| IV Sedation | Moderate–Deep | Semiconscious | Severe anxiety, long procedures |
| General Anesthesia | Full Unconsciousness | None | Surgery, complex reconstructions |
How does conscious sedation differ from other dental sedation techniques?
Definition and awareness level
Conscious sedation is a technique in which the patient is in a deeply relaxed state, yet still able to respond to verbal commands or gentle touch. It's a middle ground between minimal sedation and general anesthesia.
This differs from deep sedation or general anesthesia, where awareness is significantly reduced or eliminated.
Common uses
- Dental fillings, crowns, and extractions
- Periodontal treatments
- Procedures in patients with mild to moderate anxiety
Benefits over more profound sedation
- Lower risk profile
- Faster recovery time
- Avoids complete loss of control or awareness
- Suitable for most age groups
Comparison table
| Feature | Conscious Sedation | Deep Sedation | General Anesthesia |
|---|---|---|---|
| Awareness | Partial | Minimal | None |
| Memory of Procedure | Fuzzy or partial | Very limited | None |
| Monitoring Level | Standard dental equipment | Advanced monitoring | Hospital-level |
| Suitable For | Most dental procedures | Lengthy or invasive care | Complete surgery or extreme fear |
| Risk Level | Low | Moderate | Higher |
Is nitrous oxide still a safe and effective choice in modern dentistry?
A brief history of nitrous oxide
Nitrous oxide, often called "laughing gas," has been used in dentistry since the mid-1800s. First introduced for pain relief and mild sedation, it became popular due to its rapid onset, minimal side effects, and easy reversibility.
Despite being one of the oldest sedation methods, it remains highly relevant and widely used in modern dental practices — including in Canada.
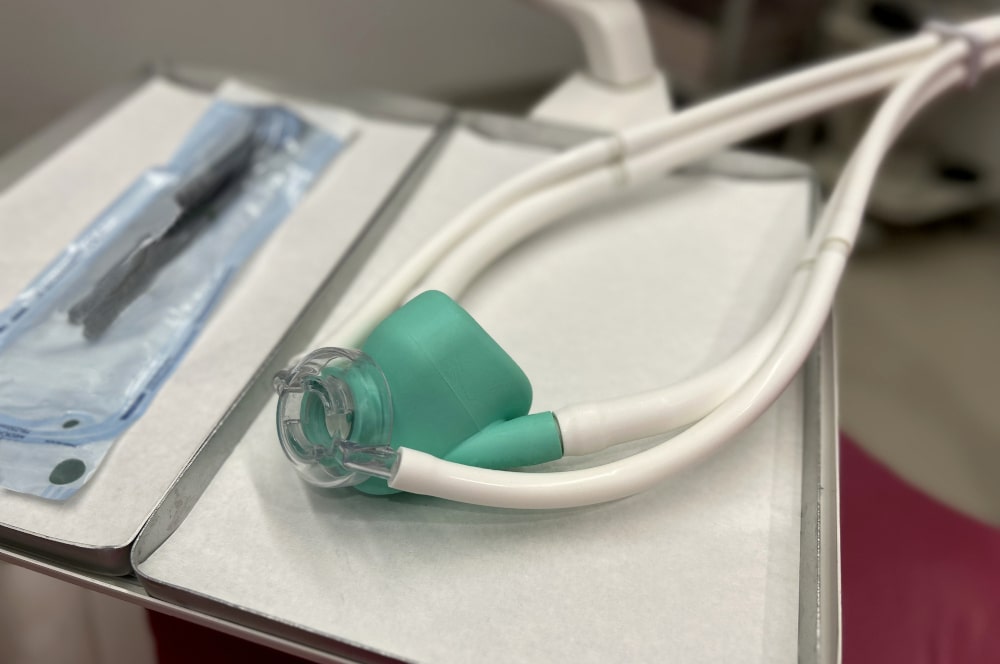
How it’s administered
Nitrous oxide is delivered through a small nasal mask. Patients inhale a precise mixture of nitrous oxide and oxygen, which takes effect within minutes.
The dentist controls the ratio and can adjust it at any time during the procedure. After the treatment, 100% oxygen is administered to flush out any remaining gas.
How fast does it work, and how fast does it wear off?
- Onset: 2–3 minutes
- Duration: Continues as long as gas is inhaled
- Recovery: 3–5 minutes with oxygen post-treatment
Patients can usually drive themselves home and return to normal activities almost immediately.
Safety profile in modern practice
According to the Canadian Dental Association (CDA):
"Nitrous oxide remains one of the safest sedation options available when administered by trained professionals. Its effects are mild, predictable, and rapidly reversible."
Nitrous oxide is exceptionally safe because:
- It doesn’t affect heart rate or blood pressure significantly
- It’s non-allergenic and non-irritating
- It has minimal interaction with other medications
- There’s no need for fasting or special preparation in most cases
Who should avoid it?
Nitrous oxide is not suitable for:
- Patients with chronic obstructive pulmonary disease (COPD)
- Pregnant individuals (especially in the first trimester)
- Those with a history of substance abuse
Specification table for nitrous oxide
| Factor | Nitrous Oxide Sedation |
|---|---|
| Delivery | Inhalation via nasal mask |
| Onset Time | 2–3 minutes |
| Recovery Time | 3–5 minutes post-oxygen flush |
| Level of Sedation | Minimal to mild |
| Consciousness | Fully conscious |
| Patient Memory | Clear (some blurring possible) |
| Monitoring Required | Light (pulse oximetry) |
| Can you Drive After? | Yes, in most cases |
| Common Uses | Pediatric dentistry, mild dental anxiety |
How do dentists ensure safety during sedation procedures?
Pre-assessment protocols
Before any sedation procedure, dentists perform a thorough medical evaluation that includes:
- Medical history and current medications
- Allergies and past surgical experiences
- Blood pressure, heart rate, and oxygen levels
- ASA (American Society of Anesthesiologists) physical status classification
Only patients who meet specific health criteria are approved for in-office sedation. High-risk patients may be referred to hospitals or specialists.
Monitoring during sedation
Dentists use advanced equipment to monitor patient vitals continuously.
- Pulse oximeter for oxygen saturation
- Blood pressure cuff with automatic readings
- ECG (for more profound sedation)
- Capnography (for tracking exhaled CO2 during IV sedation)
Many Canadian provinces require two qualified staff members during sedation procedures — one to perform the procedure and one to monitor the patient.
Certifications and training
Only dentists with specialized training and certification can offer sedation. For example:
- Dr. Amir Guorgui holds MACSD certification (Master in College of Sedation Dentistry)
- Sedation courses must be accredited and include both coursework and hands-on experience
- Offices must comply with provincial regulations and inspections
What should patients do before and after being sedated at the dentist?
Before sedation: How to prepare
Proper preparation is essential for safety and comfort. Dentists provide personalized instructions based on the sedation type, but standard protocols include:
- Fasting instructions:
- Oral or IV sedation: No solid food for at least 6 hours before the procedure
- Clear liquids (like water or apple juice) may be allowed up to 2 hours before
- Nitrous oxide: Usually, no fasting is required
- Medication management:
- Inform the dentist of all medications and supplements
- Continue prescribed medications unless instructed otherwise
- Avoid alcohol, caffeine, and recreational drugs for 24 hours prior
- Escort arrangements:
- Patients receiving anything beyond nitrous oxide must bring a responsible adult to accompany them home
- Driving post-procedure is strictly discouraged
- Wear comfortable clothing:
- Loose sleeves for IV access
- Minimal jewellery or makeup (to aid monitoring devices)
- Confirm health status:
- Reschedule if you develop a cold, fever, or respiratory issues
After sedation: What happens next?
The effects of sedation can linger for a few hours. Post-care instructions are crucial to avoid complications and support healing:
- Supervised rest:
- Rest quietly at home for the next 12–24 hours (varies by sedation level)
- Avoid strenuous activity, driving, or decision-making
- Hydration and diet:
- Begin with clear liquids, then progress to soft foods as tolerated
- Avoid alcohol and tobacco for 24 hours
- Pain or discomfort:
- Over-the-counter medications may be recommended for soreness
- Cold packs help reduce swelling after surgical procedures
- Monitoring side effects:
- Mild nausea, dizziness, or dry mouth are common
- Call the dentist if symptoms persist beyond 24 hours or worsen
- Follow-up:
- Attend any follow-up appointments to check healing and discuss future care
What should you know before choosing dental sedation?
Choosing the appropriate type of sedation is a personal decision that should be guided by your medical history, comfort level, and the complexity of the dental procedure.
Recap table of sedation methods
| Sedation Type | Awareness Level | Common Uses | Recovery Time |
|---|---|---|---|
| Nitrous Oxide | Fully awake | Children, mild anxiety | Minutes |
| Oral Sedation | Drowsy but conscious | Moderate fear, simple procedures | Hours |
| IV Sedation | Semi-conscious | Severe anxiety, lengthy procedures | Several hours |
| General Anesthesia | Unconscious | Complex surgery, special needs | Longer (hospital-based) |
Final decision-making tips
- Discuss your health history and medications openly with your dentist
- Ask whether the clinic follows certified monitoring standards
- Know your recovery plan and arrange for post-procedure supervision
- Don’t hesitate to ask for clarification on sedation levels, risks, or effects
Sources used in this article
- Canadian Dental Association – Sedation Guidelines
- Ontario Dental Association – Sedation Handbook
- Canadian Dental Regulatory Authorities Federation
- Allonfourdentalimplants.ca
FAQ
What is sedation dentistry?
It’s the use of medication to help patients relax during dental procedures. Depending on the method, patients may remain fully awake, drowsy, or deeply relaxed.
Is sedation the same as being put to sleep?
No. Most dental sedation methods are conscious sedation, where the patient remains responsive but calm, with little or no memory of the procedure.
Who should consider sedation dentistry?
Sedation dentistry is ideal for people with severe dental anxiety, low pain tolerance, a sensitive gag reflex, or those undergoing lengthy procedures.
Can children receive sedation at the dentist?
Yes, but typically only mild sedation like nitrous oxide is used for children, under strict safety protocols.
What are the most common types of dental sedation?
The main types include nitrous oxide, oral sedation, IV sedation, and general anesthesia — each varying in intensity and recovery time.
How long does dental sedation last?
Nitrous oxide wears off within minutes, oral and IV sedation last for hours, and general anesthesia requires a full recovery period.
Is sedation dentistry safe?
Yes. When performed by trained professionals, sedation is safe and closely monitored according to Canadian dental regulations.
What should I do before and after being sedated?
You may need to fast, avoid alcohol or caffeine, and arrange a ride home. Afterward, rest, hydration, and soft foods are recommended.


